URETHROPLASTY

STRICTURE URETHRA
A urethral stricture occurs when scarring narrows the tube that carries urine out of your body. Urethral stricture restricts the flow of urine from the bladder and can cause a variety of medical problems in the urinary tract, including inflammation or infection.

URETHROPLASTY
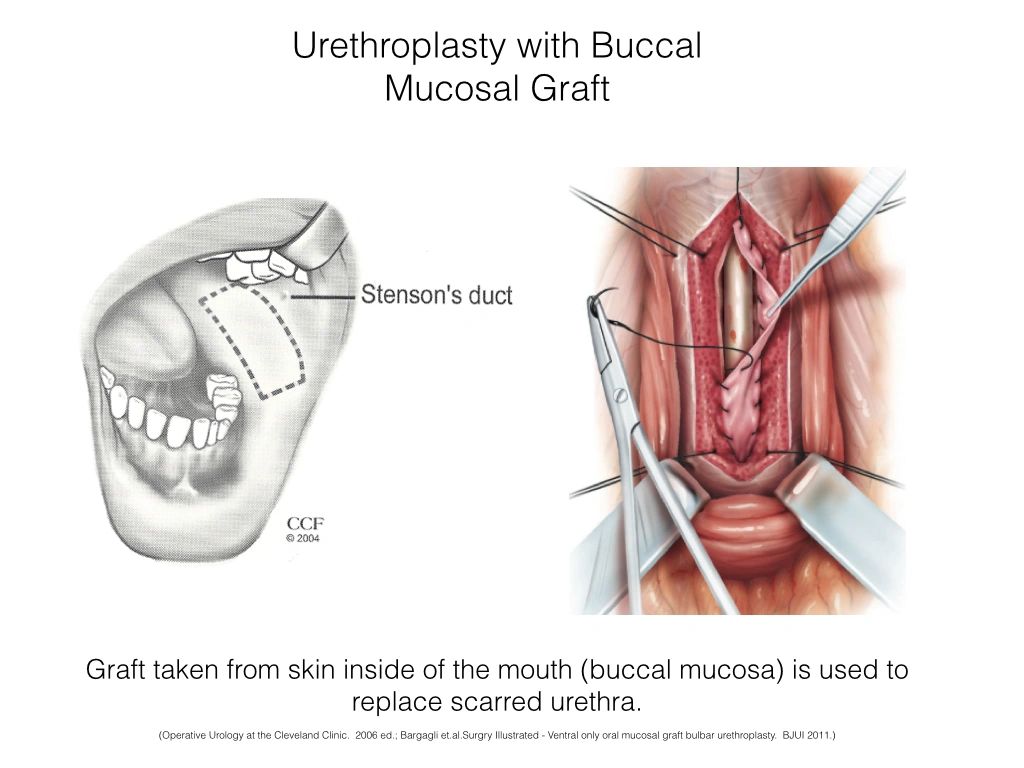
Urethroplasty involves surgically removing the narrowed section of your urethra or enlarging it. The procedure to cure urethral stricture may also involve reconstruction of the surrounding tissues. Tissues from other areas of the body, such as your skin or mouth (buccal mucosa ), may be used as a graft during reconstruction.
If done beautifully, a well-done urethroplasty of urethral stricture can save you years in medical costs and procedures. The first surgery is the best surgery. So, be aware of choosing a surgeon or surgery which promises you the easy way out, may not be a prudent decision.
ENDOSCOPIC LASER/COLD KNIFE URETHROTOMY
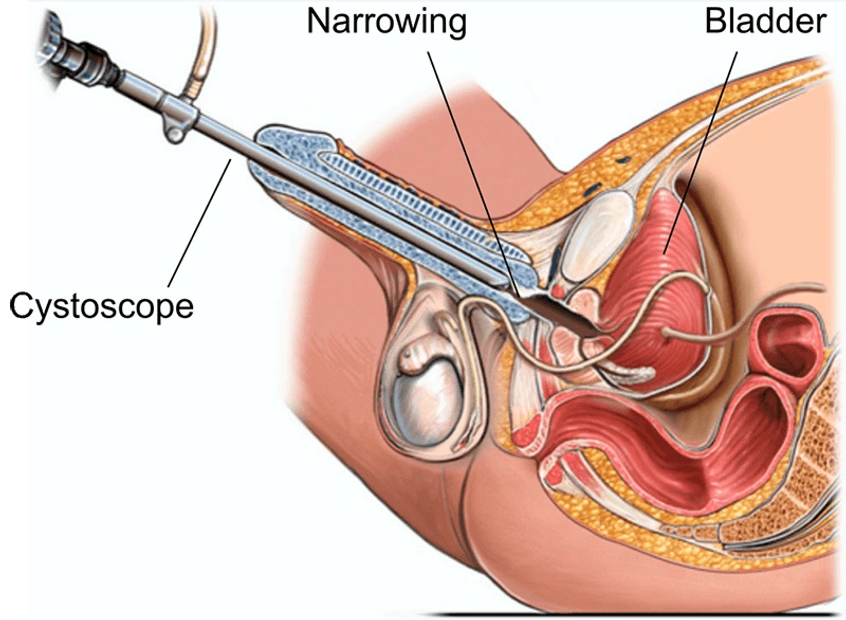
Optical Internal Urethrotomy is used to treat urethral strictures, a medical condition when the urethra (the tube that drains urine from the bladder) becomes narrow. In this surgical process, the body tissues in the urethra are CUT to release it.
BUCCAL MUCOSAL GRAFT URETHROPLASTY
Urethroplasty
What is a urethroplasty?
“Urethro” (urethra) + “plasty” (to fix) = to fix the urethra
Urethroplasty is an open surgical reconstruction or replacement of the urethra that has been narrowed by scar tissue and spongiofibrosis (urethral stricture). Urethroplasty is the gold standard for urethal reconstruction with the best and most durable results.
What is an excision and primary anastomosis (EPA) urethroplasty?
For short strictures that involve the bulbar urethra (the part of the urethra under the scrotum and up to the prostate), a segment of the scarred urethra can be completely excised. The two cut ends of the urethra are then sewn together.
Excising a short segment of urethra and sewing the ends together typically has the best long term surgical results – which approach 95%.
Stricture excision cannot be performed in the penile urethra or for long strictures of the bulbar urethra because there will be too much tension when trying to bring the two cut ends together. Tension on the suture line leads to surgical failure, and potentially to penile shortening and curvature.
What is a graft urethroplasty?
A graft is a piece of tissue that is transferred from one part of the body to another. A graft does not have its own blood supply, so it relies on the blood supply of the host (where it was transferred to) to survive. Grafts are used to increase the size of the narrow urethra by patching it, rather than a total replacement.
Typical grafts that are used to reconstruct the urethra are harvested from the extra-genital skin or from the inner lining of the mouth. The mouth graft is known as a “buccal graft”.
The lining of the mouth (cheek) is a wet and pliable tissue that makes an excellent substitute urethra. A sliver of tissue can be easily removed with no consequences. Pain is minor and feels the same as when one accidentally bites his inner cheek. The mouth heals very quickly – usually in less then 1 week.
How suceessful is graft urethropalsty?
Grafts are highly successful in the bulbar urethra as an onlay or patch technique. The lining of the cheek is typically used as a patch graft because it is easy and quick to harvest, has a hidden suture line, does not contract much, and can result in durable success rates that approach 80-85%.
Skin grafts used in urethral reconstruction can shrink as much as 50 percent, and thus result in lower success rates then the buccal graft. Penile skin should be avoided as a graft when the penile skin is not very redundant and elastic, or when the penis is affected by Lichen Sclerosus (a skin disease).
What is penile flap urethroplasty?
A flap is a transfer of tissue from one part of the body to another, where the donor blood supply is left intact.
Penile flap urethroplasty uses a flap of penile skin to reconstruct a urethral stricture that does not rely on the scarred urethra for its survival. Penile skin flaps are good for reconstructing long strictures of the penile urethra. Penile skin flaps are versatile and are used as a patch to the narrow urethral segments. Success rates in the short term approach 80-85%. Flaps that are rolled into a tube have nearly a 50 percent failure rate – so flaps are reserved for patching and not replacement.
Skin flaps from the scrotum should be avoided in urethroplasty, as their complication rate is high and their success rates poor.
What is a staged urethroplasty?
For patients who have failed prior urethroplasties, or where the urethra and local skin are severely scarred, a staged urethroplasty is usually indicated.
Here, the scarred urethra is typically surgically excised, and in its place, a buccal or skin graft is placed. This replaced urethra is left open to the air to heal over the next few months. The meatus (pee hole) is often placed in front or under the scrotum causing patients to sit to urinate for a few months. Once the graft is soft and well healed, the patient undergoes a second (‘staged”) surgery to roll the graft up into a tube to reconstruct the urethra. A staged urethroplasty can require more than two steps and more than one phase of grafting. Staged urethroplasty is typically reserved for the worst urethral strictures.
When should a urethroplasty be performed?
Before any urethroplasty, the scar should be stable and no longer contracting. Thus, it is preferred that the urethra not be dilated or cut for three months before planned definitive surgery. If the stricture patient goes into urinary retention prior to his surgery date, a suprapubic tube is typically placed. A suprapubic tube, also known as a SP tube, is a small tube that is placed through the skin and straight into the bladder. The tube is typically 2 to 3 cm above the pubic bone.
How much pain is experienced after surgery?
As with most surgeries, the pain is worst in the first 12 hours and then gradually subsides. By the morning after surgery, you should feel pretty comfortable. The pain is typically just a constant ache that lasts a few days.
If you experience sudden pain in the penis, pubic bone or lower abdomen, this is “bladder spasm” or pain from the catheter. This is not pain from your surgery. To treat the “bladder spasm” pain you can take medicines that calm the bladder down, like Ditropan, Levsin or Detrol.
How long does the surgery take?
Surgery time varies because each surgery and patient is unique. In general, the procedure takes three hours, but it can range from 2 to 5 hours, depending on the severity of the scar tissue and the extent of the reconstruction.
What should I do if I keep getting erections with the catheter in?
Erections will typically not injure or compromise the surgery, as most people will lose the erection as soon as they have pain. However, if the erections keep waking you from sleep or cause a lot of pain, then medicine can be prescribed to suppress erections.
When can I resume work?
We recommend that you allow 3 to 4 weeks off from work, especially if you do manual labor or lift heavy objects for a living. In general, it is safe to go back to work once the catheter is removed. If you have a desk job, however, you can probably return to work after 1 to 2 weeks. We suggest that you consider working shorter days the first week you return to work.
When can I resume exercise?
You can resume strenuous exercise 4 weeks after surgery. Bicycling and horseback riding are highly discouraged.
When can I resume sexual activity?
You can begin as soon as the Foley catheter is removed. If you have any new onset problems with erections, please tell your doctor.
